A 13-year-old girl in British Columbia who was hospitalized with bird flu for several weeks late last year harbored a mutated version of the virus, according to a report published this week in the New England Journal of Medicine.
The case was Canada’s first recorded human infection of avian influenza, which has infected at least 66 people in the United States since last March, according to the Centers for Disease Control and Prevention. This includes the country’s first serious case, which occurred in Louisiana in December.
So far, almost all cases of bird flu in North America have been mild, with symptoms including conjunctivitis or conjunctivitis, and a runny nose, chills, cough and sore throat.
“I think it’s concerning, but not totally surprising, that we see some sporadic cases of severe disease. Even seasonal influenza can occasionally cause very severe illness,” said Dr. Chanu Rhee, an infectious diseases and critical care physician at Brigham and Women’s Hospital and associate professor of population medicine at Harvard Medical School.
For now, the Canadian teenager and the Louisiana patient are outliers, but the infections illustrate the virus’s ability to cause severe disease and demonstrate how, during long-term illnesses, the virus has the chance to mutate to better infect humans.
In both cases, samples of the virus showed that once it was in the body, it mutated in a way that allowed it to attach to cells in the mucous membrane lining the upper respiratory tract.
“The average bird flu virus is not very good at sticking to the cells of our mucous membrane, which is what it needs to cause a human infection,” said Dr. William Schaffner, a professor of infectious diseases at the School of Medicine. Vanderbilt University. of Medicine.
Still, the presence of these mutations does not mean that the virus can definitely be transmitted from person to person.
“Just because there are mutations that could allow it to be transmitted between people doesn’t mean that’s the case,” said Angie Rasmussen, a virologist at the Vaccines and Infectious Diseases Organization at the University of Saskatchewan.
In both cases, no one else was infected, meaning the mutations do not appear to allow the virus to spread between humans, Rasmussen said.
Rhee, Rasmussen and Schaffner were not involved in any of the patients’ cases.
viral roulette
The mutations in the bird flu, or H5N1, viruses that caused severe infections in British Columbia and Louisiana occurred in a protein on the surface of the virus that allows it to stick to cells: the flu equivalent of the virus’s spike protein. coronavirus. Normally, the surface proteins of the H5N1 virus are designed to bind to receptors on birds, which is why the virus is so good at infecting birds. But the mutations seen in both severe cases allowed these versions of the virus to bind to receptors on the human mucous membrane.
Viruses replicate in any body they infect, but they are more likely to do so in people who are immunocompromised or have underlying health conditions that make it harder for their immune system to fight off a virus. As the virus persists, it replicates over and over again, occasionally creating mutations that can make the virus more adept at spreading.
“RNA viruses like flu have these enzymes that basically can’t correct spelling on their own, so they make a lot of mistakes and mutations inevitably arise,” Rasmussen said.
In addition to a mutation on the surface of the virus that allowed it to better infect humans, the British Columbia teen’s virus sample contained a mutation that allowed it to replicate rapidly once it infected cells, something the patient’s virus sample of Louisiana did not. have.
More worrying than these mutations, however, is that the virus infects humans at the same time as seasonal flu increases, Rasmussen said.
“If you get infected with H5N1 and at the same time you get infected with seasonal flu, it’s like mixing two decks of cards when they replicate, that can be extremely dangerous,” he said.
This phenomenon is called rearrangement. The 2009 swine flu outbreak is believed to have resulted from a recombination between avian, swine and human flu viruses.
“We already know that recombination is sometimes really beneficial for the virus and allows it to make a big evolutionary leap much faster than random mutations. That’s why mutations don’t worry me as much as the growing number of cases in humans,” Rasmussen said.
He compared the possibility that a virus could create a pandemic to playing the lottery.
“Many times worrying about whether a pandemic will emerge from this is like buying a lottery ticket. The odds are low, but if you buy enough tickets, eventually you will have a winner,” he said.
As the virus infects more humans, especially if those cases are not closely monitored, it creates more opportunities for the virus to mutate and mix with other viruses that are already good at infecting people.
“We’re basically giving the virus a lot of lottery tickets,” Rasmussen said.
serious illness
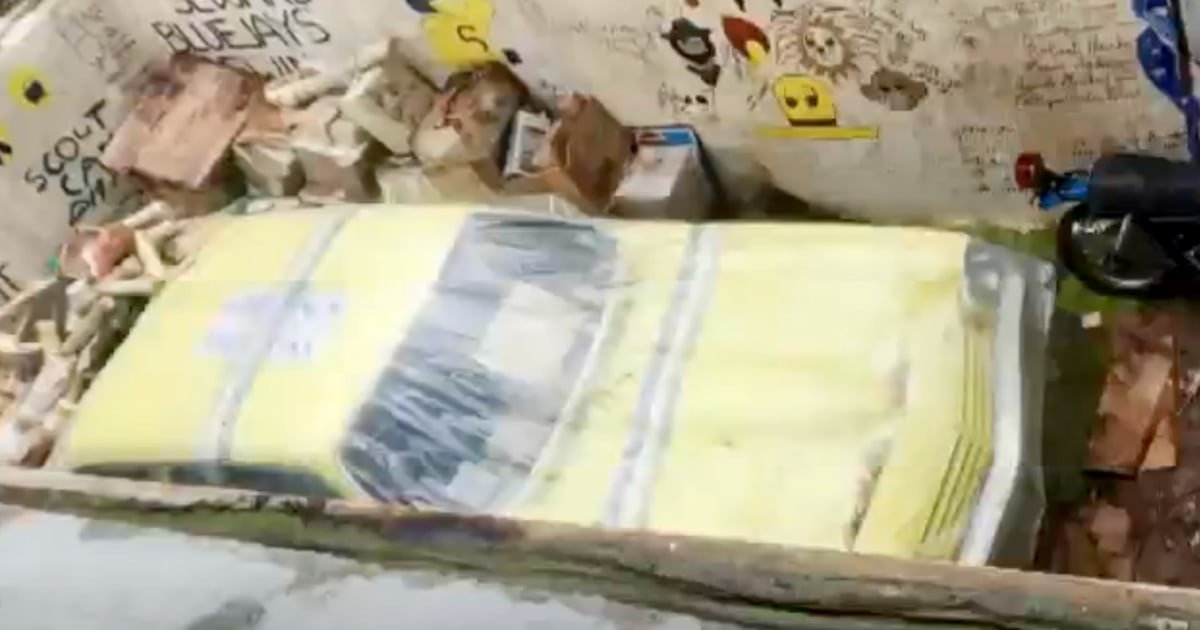
It’s still unclear where or how the Canadian girl was infected, but the version of the virus she had was “most closely related to viruses detected in wild birds in British Columbia around the same time,” according to the new report.
The Louisiana patient is also believed to have been infected by exposure to birds, in that case, a backyard flock. Other cases in the US have occurred from exposure to dairy cows or poultry.
“We are surrounded by wild animals much more than we realize,” Rasmussen said. “We are close to their feathers and their droppings. My suspicion was that it was probably a bird contact that the person didn’t realize, but how that person became infected may never be known.”
The girl, who had mild asthma and obesity, first went to the emergency room on Nov. 4 for conjunctivitis and fever, but was sent home without treatment, according to the report.
However, he continued to get sick and soon developed cough, vomiting and diarrhea.
Three days later, he returned to the emergency room: he was having trouble breathing and his body couldn’t get enough blood to his organs. The next day, November 8, she was transferred to the pediatric intensive care unit for respiratory failure, pneumonia, kidney injury, and low platelet and white blood cell counts. On Nov. 9, doctors put her on a ventilator to help her breathe and on extracorporeal membrane oxygenation, or ECMO, a life-saving machine that circulates and oxygenates blood when the lungs and heart aren’t working properly.
“That’s certainly a marker of very serious illness,” Rhee said.
The rest of the month was a blur of daily antiviral treatments and keeping the girl intubated until finally, on Nov. 28, her breathing tube was removed when doctors determined she could breathe on her own. Tests revealed that the virus, even with its mutations, was not resistant to available antivirals.
“This virus, like all other avian flu viruses, fortunately remains susceptible to the antivirals we have available,” Schaffner said.
Whether humans have immunity to bird flu is complicated and depends on a number of factors, including the strain of flu with which a person was first infected in their life, Rasmussen said.
“Viral immunologists believe there may be some cross-protection that we’ve had from previous experiences with influenza viruses, but if so, it won’t be much,” Schaffner said.