A Winnipeg sepsis survivor says he wants Manitoba to follow Nova Scotia’s lead and change the way it treats the condition that nearly killed him nine years ago.
“I came out of this in many ways a better person, but it was a huge toll on me and my family over a period of time,” Mac Horsburgh told CBC News.
Horsburgh collapsed after a cyst on his finger was misdiagnosed as inflammation and went untreated for days. The infection entered his bloodstream, weakened a vessel and created an aneurysm that ruptured.
At the time he was experiencing the most severe stage of sepsis: an extreme physical response to an infection that can cause organ failure, tissue damage and death.
Horsburgh’s doctors told his family they were not optimistic he would live. But after surgery, 10 days in a coma, three weeks in an intensive care unit and more than a week in a recovery unit, Horsburgh was discharged.
“I was ecstatic to be alive, but at the same time infuriated that a simple infection in my finger could create this type of trauma for me and my family,” he said.
For years, Horsburgh didn’t know that sepsis was what almost killed him, and he has since learned that it could have been prevented if the infection had been treated sooner.
“Health care services saved my life, but medical care in the early stages also created the problem for me,” he said. “I’ve struggled with the idea that we’re not doing enough for sepsis patients.”
But with a recent plan in Nova Scotia to speed up sepsis treatment, Horsburgh sees an opportunity for change in Manitoba, too.
Changes in Nova Scotia
Nova Scotia’s health system is transitioning to allow nurses and paramedics in emergency rooms and urgent treatment centers to begin a course of antibiotics, without a doctor’s order, for a patient believed to have sepsis.
Nova Scotia emergency rooms once had the ability to medicate sepsis patients shortly after triage, but that is no longer the case due to increasing wait times, said Dr. Vanessa Sweet, an anesthesiologist and co-director of the province’s sepsis action improvement plan.
Nova Scotia began testing its new sepsis response in July 2024 and rolled it out across the province in September.
The hope is to speed up response times to treat the disease, which Sweet said has become a key cause of hospital deaths in the province.
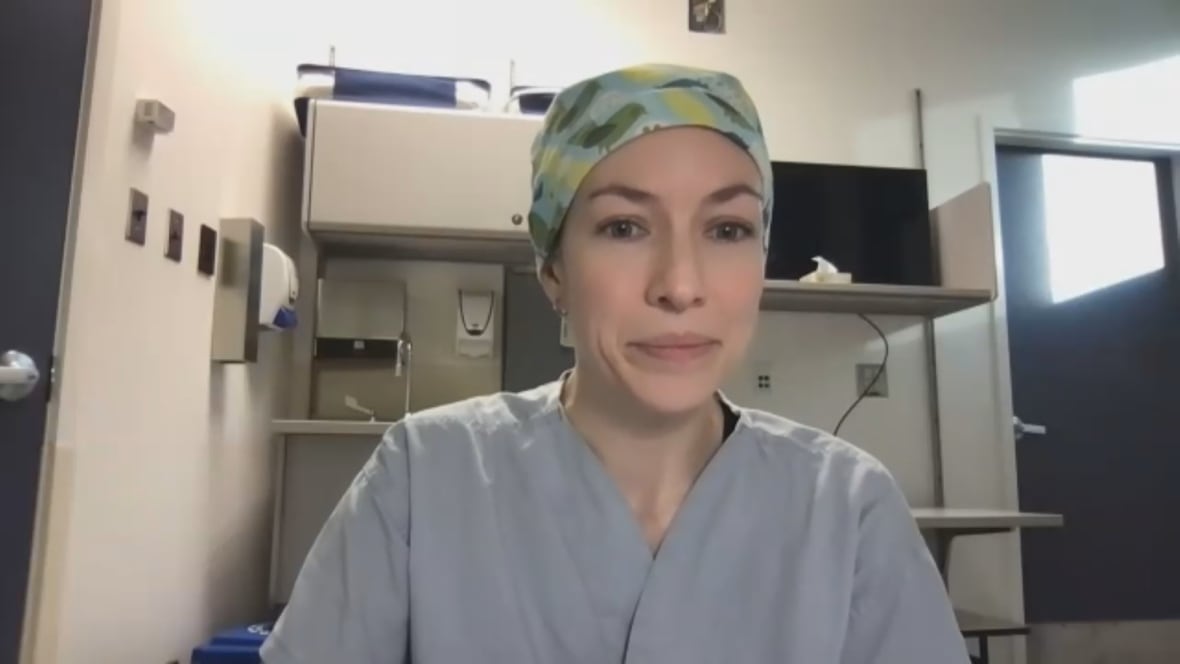
“The sooner we can move that critical piece in a patient’s journey in the emergency department, the better,” he said.
“You can reach a situation where blood pressure drops dangerously and various organs begin to not function.”
Nova Scotia has also equipped health centers with sepsis treatment kits, in addition to introducing a standardized protocol to detect the disease.
The province is also now providing information packs for sepsis patients during recovery, something Horsburgh said would have helped him when he was discharged, with little information.
“My life had become a big puzzle, but I was missing many pieces,” he said.
‘Actions speak louder than words’
TOAccording to the Canadian Sepsis Foundation, one in every 18 deaths in Canada is related to sepsis, making it the 12th leading cause of death nationally.
It is one of the most common reasons for admissions to Winnipeg intensive care units, says infectious diseases and critical care doctor.
While the sickest patients with sepsis receive treatment almost immediately, those with a mild degree of infection usually have to wait longer in the emergency room for a doctor to prescribe antibiotics, said Dr. Sylvain Lother.
But giving nurses and paramedics, who are usually the first to detect the disease, the power to start treatment early could help prevent serious complications in patients with moderate infection, he said.
“Doing testing more quickly and starting treatment right away could make symptoms improve much faster,” Lother said.

But any change must be accompanied by staff training and protocols so that the proper medication is administered, he said.
“If we prescribe an antibiotic that’s not… potent enough, it doesn’t kill the bacteria. We know that’s associated with almost doubling the risk of mortality,” Lother said.
“On the other hand, overuse of antibiotics leads to organisms that are resistant, and then we have problems… where future infections may be more difficult to treat.”
In Manitoba, nurses can initiate lab tests to detect sepsis when it is suspected in the emergency room, according to Shared Health. But antibiotics or intravenous treatment must be ordered by a physician, physician assistant, nurse practitioner, or clinical assistant before they can be administered.
A spokesperson for the health minister said the province is focused on ensuring all sepsis patients receive the same treatment across Manitoba.
The province is looking to expand who can prescribe sepsis medications in the future, the spokesperson said, but did not give a timeline.
The Manitoba Nurses Union is in favor of allowing nurses to order sepsis medications.
“Just like a stroke, timing is very important,” said union president Darlene Jackson. “If you can start those procedures and those protocols quickly, then your patient has a better chance of making a full recovery.”
Horsburgh is encouraged that the province is exploring options to improve sepsis care, but his optimism is cautious.
“Words are one thing,” he said. “Actions speak louder than words. So I’m still going to wait and see.”
Mac Horsburgh, who nearly died from sepsis, wants Manitoba to improve treatment and screening. Nova Scotia recently began allowing nurses and paramedics to start antibiotics for the most serious infections in the emergency department without a doctor’s order.